Skin cancer is the most common type of cancer worldwide—and it is on the rise, especially in sunny regions like the Middle East. It happens when abnormal cells grow uncontrollably in the skin. While most skin cancers are treatable when caught early, some types can be life-threatening if diagnosed or treated late.
While there are many types of skin cancer, the three main types of skin cancer:
While most skin cancers are common and treatable, some rare types require specialized care. Dermatofibrosarcoma protuberans (DFSP) is a slow-growing tumor that starts in the deep layers of the skin and can spread if not treated early. Merkel cell carcinoma (MCC) is a fast-growing and aggressive cancer that often appears as a painless bump on sun-exposed areas, especially in older adults. Cutaneous T-cell and B-cell lymphomas are cancers of the immune system that affect the skin, causing patches, plaques, or nodules that may resemble eczema or psoriasis. These rare cancers need expert diagnosis and advanced treatment plans to ensure the best outcomes.

Skin cancer develops due to a mix of environmental and genetic factors. Here are the key contributors:
Early detection saves lives. Skin cancer often starts as a small change on the skin—something you might overlook unless you know what to watch for.
Here are the key warning signs:
Use the ABCD rule to spot suspicious changes of existing or new moles
If you notice any unusual changes, consult a dermatologist promptly. Most skin issues are harmless—but only a medical exam can confirm that.
At Skin Experts Polyclinic in Dubai, we follow a thorough and precise approach to diagnosing skin cancer. Early and accurate diagnosis is key to successful treatment.
At Skin Experts Polyclinic, we use the FotoFinder ® system, a cutting-edge device that combines automated total body mapping with digital dermoscopy. This technology captures high-resolution images of the entire skin surface and individual moles, allowing us to monitor even the smallest changes over time. FotoFinder helps our dermatologists —making skin checks faster, safer, and more precise for every patient. FotoFinder is a good documentation tool, although experience and clinical examination remains the most important factor in determining the risk of a lesion.
If a lesion looks suspicious, we recommend a biopsy to evaluate it histopathologicaly.
At Skin Experts Polyclinic, we offer advanced and personalized treatments for all types of skin cancer. The choice of treatment depends on the type, size, location, and depth of the cancer. Our goal is to remove the cancer completely while preserving healthy skin and achieving excellent cosmetic results.
This is the most common treatment for basal and squamous cell carcinomas located on the trunk or the extremities.
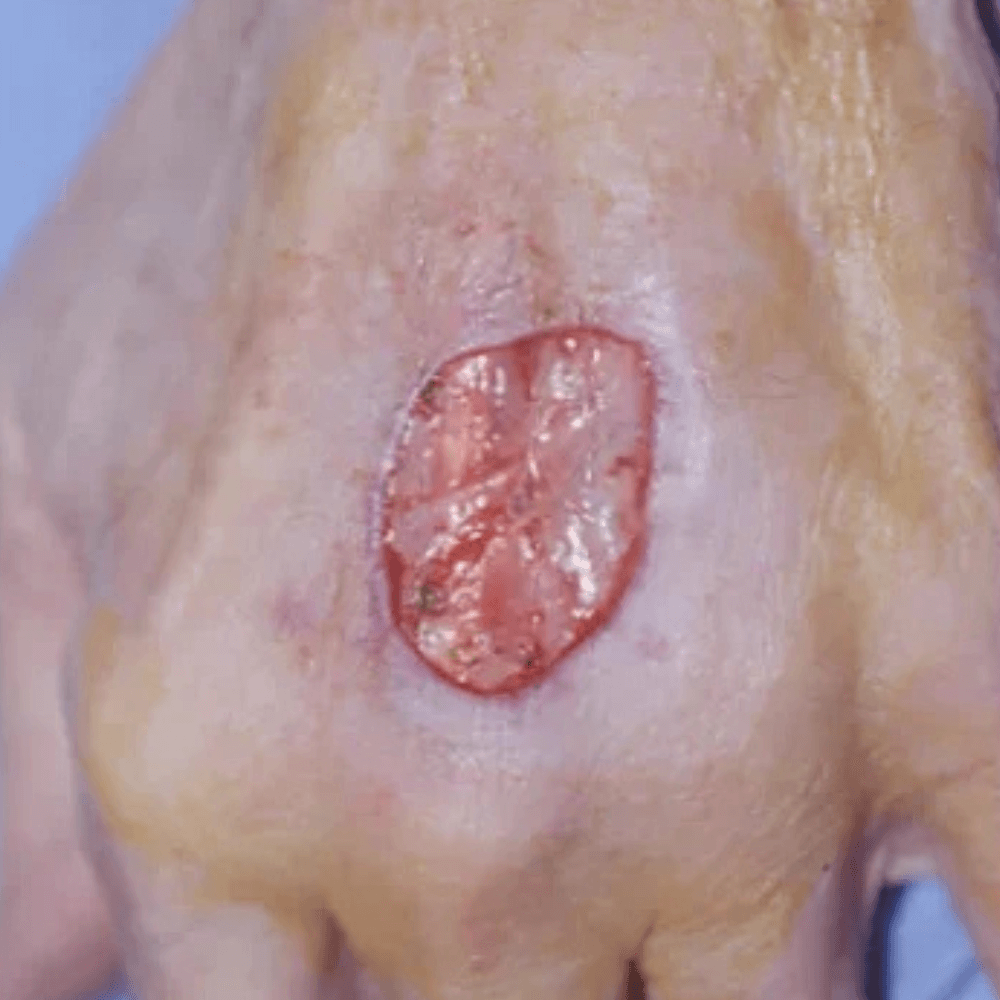
Mohs Micrographic Surgery is the best way to treat skin cancer in delicate areas like the face, lips, or around the eyes, for recurrent cancers, young people, or whenever a minimal scar is desired.
We use Mohs surgery, the gold standard in precision skin cancer removal:
Photodynamic Therapy (PDT) is a non-invasive treatment used for certain types of skin cancer, including superficial basal cell carcinoma, Bowen’s disease, and defuse actinic keratosis. It works by applying a special light-sensitive cream to the affected area, followed by exposure to a controlled light source. This combination activates a reaction destroying abnormal cells while leaving healthy skin untouched. PDT is especially useful for treating large or multiple lesions in cosmetically sensitive areas, offering excellent cosmetic results with minimal scarring. It’s performed in our clinic as an outpatient procedure and requires little recovery time. Dr. Touma has done major research to advance the use of PDT for precancers or cancer lesion. [1]
[1] Touma, D., Yaar, M., Whitehead, S., Konnikov, N., & Gilchrest, B. A. (2004). A trial of short incubation, broad-area photodynamic therapy for facial actinic keratoses and diffuse photodamage. Archives of Dermatology, 140(1), 33–40. https://doi.org/10.1001/archderm.140.1.33
Laser treatment is used for precancerous lesions like actinic keratoses and some superficial skin cancers:
Nd:YAG and Alexandrite laser therapy is a non-invasive option for treating select cases of low-risk basal cell carcinoma (BCC) and Bowen’s disease. This laser emits a 1064 nm wavelength that penetrates deep into the skin, targeting cancerous cells while preserving surrounding healthy tissue. Studies have shown that Nd:YAG treatment offers a low recurrence rate and excellent cosmetic outcomes, with minimal scarring and pigmentation changes. It is particularly useful for patients seeking alternatives to surgery for lesions on the body and extremities
Erbium:YAG laser therapy offers a precise, tissue-sparing option for treating precancerous actinic keratosis, superficial non-melanoma skin cancers, such as Bowen’s disease and superficial basal cell carcinoma. Operating at a wavelength of 2940 nm, the Er:YAG laser is highly absorbed by water-rich tissues, allowing for controlled ablation of cancerous cells with minimal thermal damage to surrounding skin. This makes it ideal for lesions in cosmetically sensitive areas, especially when surgical excision is contraindicated or declined. The procedure is typically performed under local anesthesia and may be combined with histologic confirmation or adjunctive topical therapies. Healing is rapid, and cosmetic outcomes are excellent, with reduced risk of scarring or pigment alteration. In our practice Erbium:YA laser has replaced cryotherapy as it is more precise and it is better and faster and avoid scaring and depigmentation seen with aggressive cryotherapy.
Depending on the case, we may also recommend:
Skin cancer is largely preventable. At Skin Experts Polyclinic, we believe that smart habits and regular skin care can dramatically reduce your risk. Here’s how to protect your skin—especially in sunny climates like the UAE:
At Skin Experts Polyclinic, we combine world-class expertise with cutting-edge technology to deliver the highest standard of skin cancer diagnosis and treatment in the UAE.
Whether you’re seeking a routine skin check or advanced cancer treatment, Dr Touma and his team are your trusted partner in skin cancer treatment.
Don’t wait for symptoms to appear—early detection saves lives. Whether you’re concerned about a mole, sun damage, or simply want peace of mind, our expert dermatology team is here to help.
Your skin deserves expert care. Let’s protect it—together.
Dr. Touma is a highly professional doctor who works with ethics and precision. I have had problems with skin cancer, and I trust that his follow up and care have been a major factor in my treatment and current well-being. He does not only care about getting the job done, but takes care of the aesthetic side as well for the sake of the patient's morale, in addition to always keeping up with new research and providing updated advice. His staff is also pleasant and professional and make you feel at home rather than in a conventional doctor's clinic.
We use local anesthesia to numb the area, so you’ll feel minimal discomfort. Most patients say it feels like a quick pinch.
Typically, within 48 hours. Our pathology partners prioritize skin cancer cases for fast and accurate diagnosis.
We carefully recommend treatment option that offers customized highest tumor Clarence and aesthetic results. Mohs surgery offers the best cosmetic outcome, especially for facial lesions. We also offer laser treatments to minimize scarring.
No. Skin cancer is not infectious and cannot be passed from person to person.
We customize treatment to make sure the risk of recurrence is minimal, and recommend regular visit to monitor our patients.
Most insurance plans cover diagnostic procedures and medically necessary treatments. Our team can assist with pre-authorization and documentation.
Depending on your risk, we may recommend a yearly full-body skin exam every 3–12 months in case of prior skin cancer, especially if you have risk factors like fair skin, frequent sunburns, or a family history of melanoma.
It’s rare, but possible—especially in children with severe sunburns and genetic predisposition. Early education and sun protection are key.
Clinical Insight: This case features a young female patient with a pearly, ulcerated basal cell carcinoma (BCC) on the upper chest—a high-visibility area requiring both oncologic precision and aesthetic sensitivity. Mohs micrographic surgery was chosen to ensure complete tumor clearance while preserving surrounding healthy skin. The intraoperative phase demonstrated meticulous margin control with minimal tissue sacrifice. Layered closure achieved excellent contour restoration and minimal scarring. This case underscores the value of Mohs surgery in cosmetically exposed zones, especially for younger patients where long-term aesthetic outcomes are paramount.
Clinical Insight: This case features a female patient with basal cell carcinoma (BCC) on the nasal bridge—a high-risk, cosmetically sensitive site. Mohs micrographic surgery was performed to achieve complete tumor excision while preserving surrounding healthy tissue. The resulting defect was reconstructed using a transposition flap, selected for its ability to restore nasal contour, maintain symmetry, and minimize scarring. The layered closure provided excellent functional and aesthetic outcomes, reinforcing Mohs surgery as the gold standard for facial BCCs.
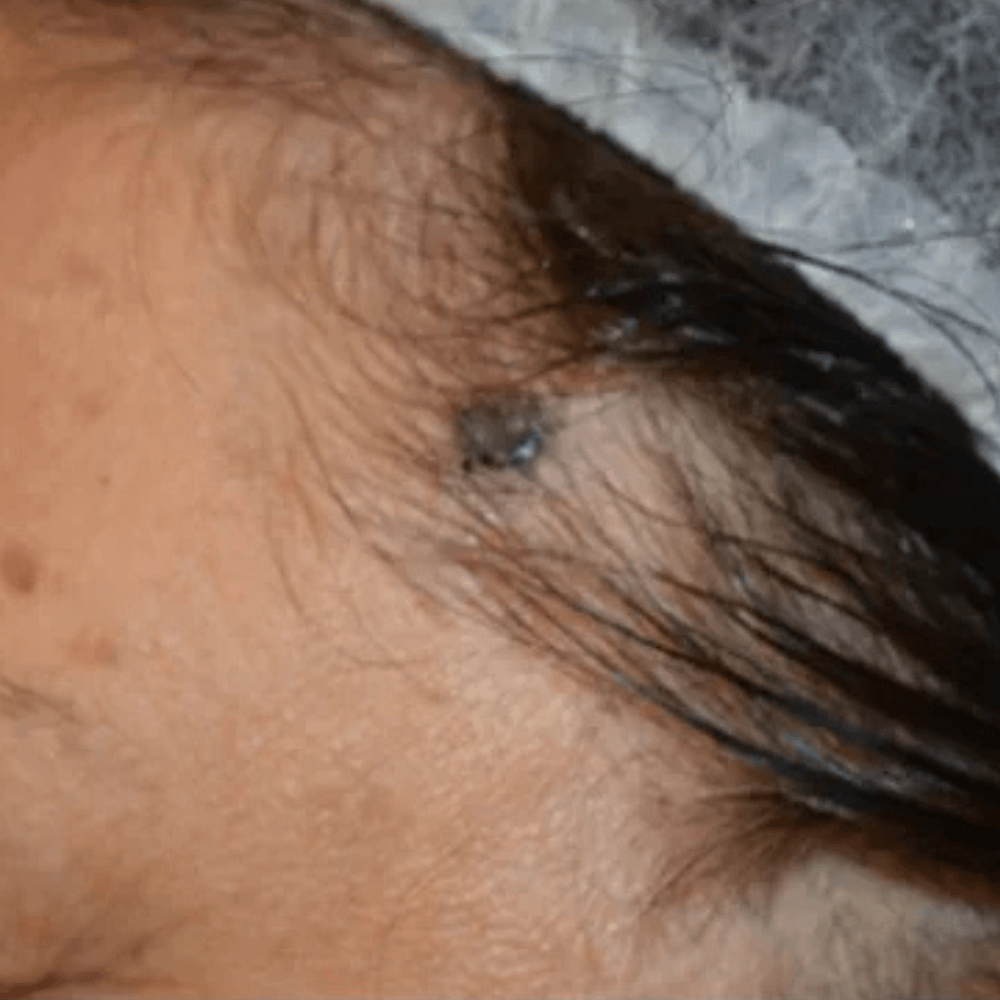
Clinical Insight: This case presents two basal cell carcinomas (BCCs) on the scalp—an uncommon but challenging site due to limited skin mobility and aesthetic considerations. The patient exhibited two ulcerated nodules in sun-exposed regions of the scalp, likely exacerbated by hair thinning and chronic UV exposure. Mohs micrographic surgery was performed to ensure complete tumor clearance with maximal tissue conservation. Layer-by-layer margin assessment confirmed full excision. Postoperative linear closures achieved excellent alignment with minimal disruption to surrounding hair-bearing tissue, highlighting the precision and cosmetic advantage of Mohs surgery in scalp BCC management.
Clinical Insight: This case demonstrates the use of full-thickness skin grafting to reconstruct a nasal tip defect following Mohs micrographic surgery for basal cell carcinoma (BCC). The lesion’s depth and central facial location made primary closure impractical. After complete tumor excision with tissue preservation, a full-thickness graft harvested from the ear bowl was used to restore nasal contour and texture. The graft achieved excellent integration with minimal architectural distortion, preserving nasal symmetry and ensuring oncologic safety in a cosmetically sensitive zone.
Clinical Insight: This case illustrates the use of a bilobed transposition flap for reconstructing a nasal sidewall defect following Mohs micrographic surgery for basal cell carcinoma (BCC). The lesion’s location—spanning the nasal sidewall and alar region—posed both oncologic and aesthetic challenges. Mohs surgery achieved complete tumor clearance with tissue conservation. A bilobed flap was selected to optimize contour restoration, color match, and structural integrity. At follow-up, the reconstruction preserved nasal symmetry with minimal scarring, underscoring the value of flap techniques over grafting in cosmetically sensitive facial zones, and the importance of a histologically confirmed clearance before such complex reconstruction is undertaken, a tumor that recurs after this type of reconstruction will grow below the flap for long before it might be seen clinically.
Clinical Insight: This case highlights a palliative treatment strategy for multiple superficial squamous cell carcinomas in situ (SCCIS) affecting the forehead and scalp of a patient with Epidermodysplasia Verruciformis (EDV)—a rare genetic disorder linked to chronic HPV susceptibility and widespread skin dysplasia. Given the extent of disease and surgical limitations, a multimodal non-invasive approach was adopted, combining curettage, blue light photodynamic therapy (BLU-U PDT), and topical Imiquimod. The baseline presentation included crusted, erythematous plaques; following treatment, the patient showed marked lesion regression and immune activation. At 4-year follow-up, the patient remained in sustained remission with no new lesions and excellent cosmetic results, demonstrating the long-term efficacy of PDT and Imiquimod in managing chronic viral-induced dysplasia.
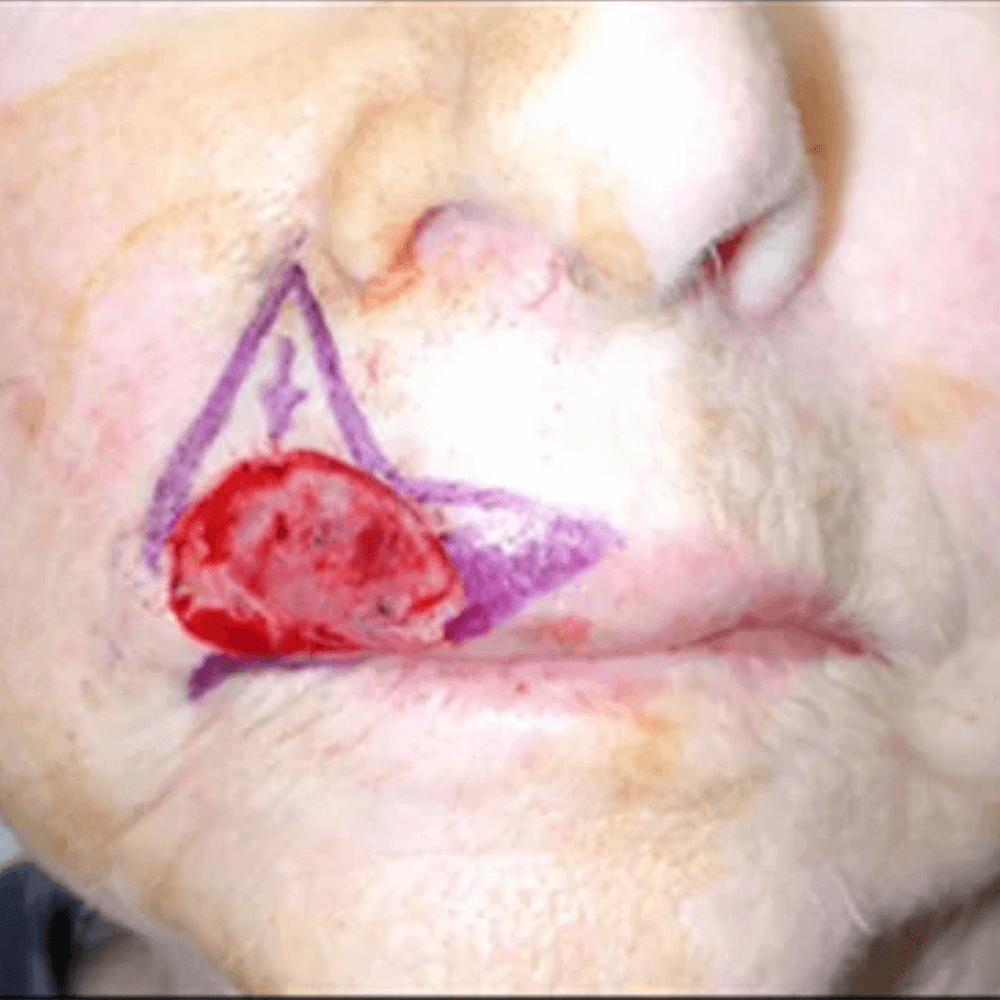
Clinical Insight: This case illustrates the successful use of intralesional methotrexate (MTX) injection for treating a rapidly growing keratoacanthoma on the upper lip of a young woman. The lesion, a crateriform squamous neoplasm with central keratin plug, posed both cosmetic and therapeutic challenges. A conservative, non-surgical approach was selected, administered over five biweekly sessions. The tumor showed progressive regression, with gradual healing and restoration of lip contour and texture. At one-year follow-up, the patient achieved complete resolution with excellent cosmetic outcome and no recurrence—highlighting MTX’s value as a minimally invasive option for keratoacanthoma in cosmetically sensitive areas.
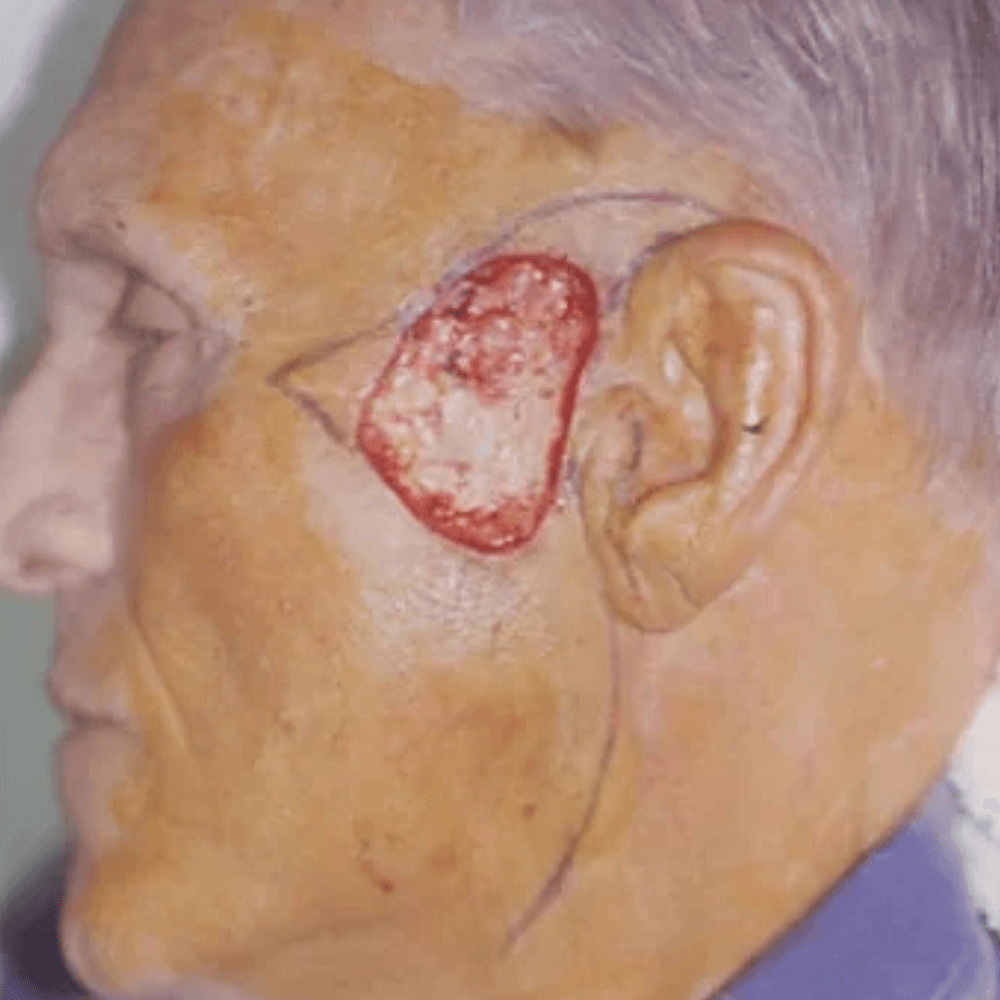
Clinical Insight: This image documents a case of recurrent lentigo maligna (LM) on the left cheek, following three prior surgical excisions. LM, a challenging subtype of melanoma in situ, often evades complete removal due to subclinical extension. After the fourth recurrence, topical Imiquimod was chosen as a field-directed immunotherapy, offering a non-invasive alternative in a surgically complex area. The treatment course illustrates Imiquimod’s immunomodulatory effect: subtle pigmentation and scarring pre-treatment, followed by intense redness, crusting, and erosion during therapy—hallmarks of immune activation. Post-treatment, the lesion resolved with no residual redness and scarring, and no clinical evidence of recurrence, highlighting Imiquimod’s potential for durable clearance in resistant LM.
Clinical Insight: This case demonstrates successful treatment of superficial basal cell carcinoma (sBCC) on the upper arm using short-pulse Alexandrite laser therapy. The patient underwent two sessions with a 3-millisecond pulse duration, targeting the lesion with precision while minimizing thermal damage to surrounding tissue. The initial presentation showed a well-demarcated erythematous plaque with central crusting. Following treatment, progressive lesion clearance was observed, with marked reduction in erythema and restoration of normal skin texture. At final follow-up, the treated area exhibited excellent cosmetic recovery with no visible scarring, highlighting the potential of Alexandrite laser as a non-invasive option for select cases of superficial BCC, that might otherwise necessitate disfiguring surgery.